Table of Contents
TLDR
Wet Brain is a colloquial term for Wernicke-Korsakoff syndrome, a serious neurological condition caused by severe thiamine (vitamin B1) deficiency, most commonly resulting from chronic alcohol misuse. This syndrome encompasses two distinct stages: Wernicke’s encephalopathy, which appears first with acute symptoms like confusion and coordination problems, and Korsakoff psychosis, characterized by severe memory impairments. Furthermore, while early intervention with thiamine supplementation can prevent progression, the condition becomes increasingly difficult to reverse once Korsakoff syndrome develops. Consequently, individuals struggling with alcohol use disorder face elevated risk, making professional treatment essential.
Introduction
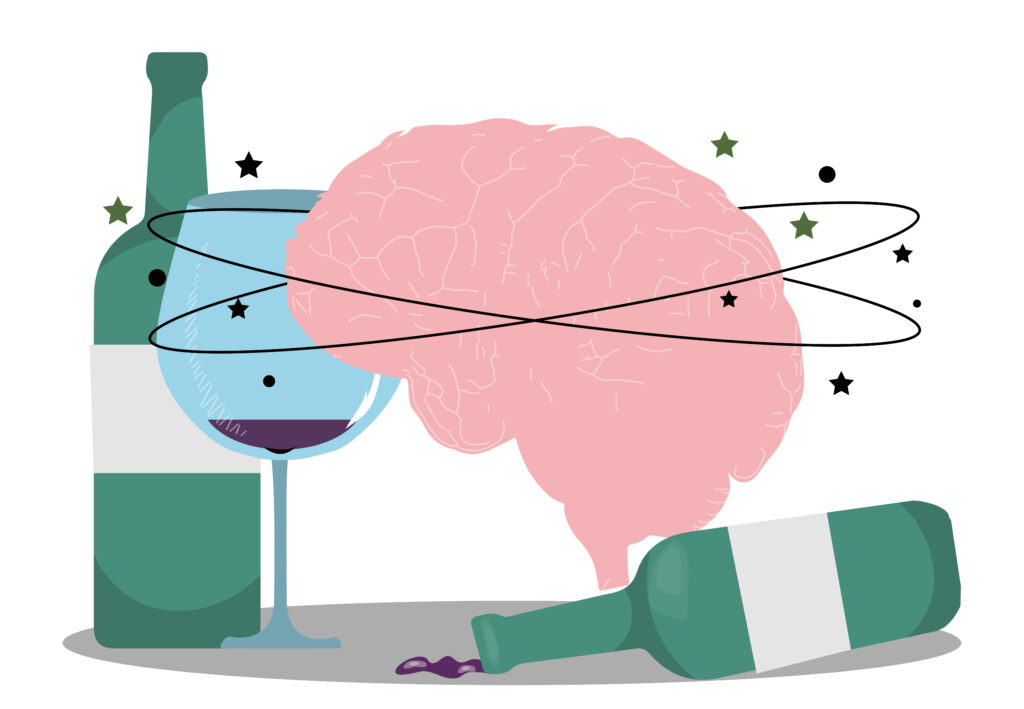
The human brain requires consistent nourishment to function properly. However, when alcohol takes precedence over nutrition, a pattern far too common among those battling addiction, the consequences extend beyond mere forgetfulness. Wet Brain represents one of alcohol’s most devastating effects, transforming vibrant minds into fragmented repositories of lost memories. This isn’t simply about having trouble recalling names; rather, it’s a profound neurological crisis demanding immediate attention and specialized care.
What Is Wernicke-Korsakoff Syndrome (“Wet Brain”)?
Wernicke-Korsakoff syndrome, colloquially known as Wet Brain, is a two-stage brain disorder resulting from severe thiamine deficiency [1]. The medical community recognizes this condition as one of the most serious complications of chronic alcohol misuse. Initially, Wernicke’s encephalopathy manifests as an acute, reversible phase characterized by neurological disturbances. Subsequently, if left untreated, it progresses into Korsakoff psychosis, a chronic and often irreversible condition marked by severe memory problems [2].
Think of thiamine as the brain’s premium fuel, without it, neural pathways sputter and fail. Moreover, the syndrome affects specific brain regions responsible for memory formation and coordination. Consequently, individuals with Wet Brain experience a cascade of neurological problems that fundamentally alter their ability to function independently.
How is Alcohol Misuse Connected to Wernicke-Korsakoff Syndrome?
Alcohol creates a perfect storm for thiamine deficiency through multiple mechanisms:
- Excessive drinking directly impairs the body’s ability to absorb thiamine from the digestive tract [3]
- Alcohol damages the liver, which converts thiamine into its active form
- Individuals struggling with addiction often neglect proper nutrition, replacing meals with drinks
- Alcohol increases thiamine excretion through urine while increasing metabolic demand
Therefore, chronic drinkers find themselves caught in a vicious cycle: their bodies need more thiamine while simultaneously becoming less capable of obtaining and utilizing it [4].
Who is at Risk for Developing Wernicke-Korsakoff Syndrome?
While anyone can develop Wet Brain under the right circumstances, certain populations face significantly elevated risk:
- Chronic heavy drinkers who have consumed excessive alcohol for years or decades
- Individuals with eating disorders that severely restrict food intake
- People undergoing dialysis or experiencing kidney failure
- Cancer patients receiving chemotherapy affecting nutrient absorption
- Those with AIDS or other conditions causing severe malnutrition
- Individuals who’ve undergone gastric bypass surgery
Notably, the syndrome doesn’t discriminate based on demographics. Nevertheless, research indicates that men develop Wet Brain more frequently than women [1]. Furthermore, individuals with untreated alcohol use disorder face exponentially higher risk.
Wernicke-Korsakoff Syndrome Symptoms
Understanding warning signs becomes crucial for early intervention and potentially reversing damage before permanent complications set in.
| Stage | Primary Symptoms | Reversibility |
| Wernicke’s Encephalopathy | Confusion, ataxia, eye problems | Potentially reversible with immediate treatment |
| Korsakoff Psychosis | Severe memory loss, confabulation | Often irreversible |
[Insert image of neurological symptom progression here]
Wernicke’s Encephalopathy Symptoms
Wernicke’s encephalopathy arrives suddenly. The classic triad includes:
- Confusion and mental disorientation that appears rapidly
- Ataxia (loss of coordination and balance) making walking difficult
- Ocular abnormalities including involuntary eye movements and double vision
Beyond this triad, patients may experience profound apathy and memory problems. In fact, approximately 80% of individuals show abnormal eye movements [2]. Additionally, some develop hypothermia or low blood pressure. Without immediate medical intervention, these symptoms progress rapidly, potentially leading to coma or death.
Korsakoff Psychosis Symptoms
When Wernicke’s encephalopathy goes untreated, it frequently evolves into Korsakoff psychosis, the chronic stage of Wet Brain syndrome bringing devastating cognitive impairments.
The hallmark symptoms include:
- Severe memory problems, particularly forming new memories
- Confabulation, unconsciously creating false memories to fill gaps
- Lack of insight into their condition
- Apathy and minimal emotional response
Interestingly, individuals with Korsakoff psychosis often appear alert and can hold conversations. However, they’ll repeat the same stories without realizing it and create elaborate but entirely fictional narratives [5]. This creates profound frustration for family members.
How is Wernicke-Korsakoff Syndrome Diagnosed?
Diagnosing Wet Brain requires comprehensive clinical evaluation. Physicians typically combine several approaches: assessing the classic symptom triad while reviewing alcohol consumption history, conducting blood tests to measure thiamine levels, utilizing neuroimaging including MRI scans, and performing cognitive assessments [3].
Early diagnosis proves critical. Therefore, medical professionals maintain high suspicion when treating anyone with known alcohol use disorder who presents with neurological symptoms.
Is Wernicke-Korsakoff Syndrome Preventable?
Absolutely, and prevention remains far more effective than treatment. The primary prevention strategy involves addressing alcohol misuse before severe thiamine deficiency develops. Moreover, healthcare providers often administer prophylactic thiamine supplementation to individuals undergoing alcohol detoxification [4].
Prevention strategies include maintaining adequate nutrition despite alcohol consumption, taking thiamine supplements as recommended, seeking treatment for alcohol use disorder before complications arise, and regular medical monitoring. Furthermore, treatment centers routinely administer thiamine to patients entering rehabilitation programs.
Is Wernicke Korsakoff Syndrome Reversible?
The reversibility of Wet Brain depends entirely on timing and treatment. Wernicke’s encephalopathy, when caught early and treated aggressively with high-dose thiamine, often improves dramatically. Specifically, eye movement abnormalities typically resolve within days [5].
However, once Korsakoff psychosis develops, the prognosis becomes considerably grimmer. Research indicates that only about 25% of individuals achieve complete recovery, approximately 50% experience partial improvement, and the remaining 25% show minimal response [1]. Nevertheless, even partial recovery can meaningfully improve quality of life.
The key factor remains early intervention. Consequently, anyone exhibiting signs requires immediate medical attention, waiting even a few days can mean the difference between recovery and permanent disability.
How is Wernicke-Korsakoff Syndrome Treated?
Treatment protocols focus on two primary objectives: replenishing thiamine and addressing underlying alcohol addiction. Medical teams administer high-dose thiamine intravenously, as oral supplementation alone proves insufficient [2].
The comprehensive treatment approach includes:
- Immediate IV thiamine replacement (often 500mg three times daily initially)
- Nutritional rehabilitation with balanced meals and vitamin supplementation
- Management of alcohol withdrawal in medically supervised settings
- Long-term alcohol treatment including therapy and medication-assisted treatment
- Cognitive rehabilitation for persistent memory problems
Additionally, patients require supportive care addressing related health issues common in chronic alcoholism. Therefore, successful treatment demands a multidisciplinary team approach.

Treatment for Alcohol Use Disorder and Alcohol Addiction at Flagler Health & Wellness
At Flagler Health & Wellness, we understand that preventing conditions like Wet Brain requires comprehensive, evidence-based alcohol addiction treatment. Our multidisciplinary team provides individualized care that addresses both the physical and psychological aspects of alcohol use disorder.
Our treatment programs include medically supervised detoxification with prophylactic thiamine supplementation, evidence-based therapies including cognitive-behavioral therapy, medication-assisted treatment when appropriate, nutritional counseling and rehabilitation, and family therapy and support services. Importantly, we recognize that each person’s journey toward recovery looks different.
Don’t wait until serious complications develop. If you or someone you love is struggling with alcohol addiction, contact us today to learn how we can help you begin the path toward lasting recovery.
Frequently Asked Questions
Q: Can you recover from Wet Brain if you stop drinking?
A: Recovery depends on the stage when treatment begins. If caught during Wernicke’s encephalopathy and treated immediately with thiamine, many symptoms can improve significantly. However, once Korsakoff psychosis develops, full recovery becomes unlikely, though some improvement remains possible with abstinence and proper nutrition.
Q: How long does it take to develop Wet Brain from alcohol?
A: There’s no specific timeline, as development depends on drinking patterns, overall nutrition, and individual physiology. However, it typically develops after years of heavy, chronic alcohol consumption combined with poor nutritional intake.
Q: What are the first signs that someone might be developing Wet Brain?
A: Early warning signs include increasing confusion, difficulty with balance and coordination, unusual eye movements, and significant memory problems. Additionally, watch for extreme apathy and confabulation. Anyone displaying these symptoms with a history of heavy alcohol use requires immediate evaluation.
Q: Can Wet Brain occur in people who don’t drink alcohol?
A: Yes, though it’s rare. Any condition causing severe thiamine deficiency can potentially lead to Wernicke-Korsakoff syndrome, including eating disorders, gastric bypass surgery, chronic vomiting, cancer, and AIDS. However, chronic alcohol misuse remains the most common cause.
Q: Is Wet Brain the same as alcohol-related dementia?
A: No, though they’re related. Wet Brain specifically refers to Wernicke-Korsakoff syndrome caused by thiamine deficiency. Alcohol-related dementia is a broader term encompassing various types of cognitive decline from chronic alcohol consumption.
References
[1] Martin, P. R., Singleton, C. K., & Hiller-Sturmhöfel, S. (2003). The role of thiamine deficiency in alcoholic brain disease. Alcohol Research & Health, 27(2), 134-142. – https://pubmed.ncbi.nlm.nih.gov/15303623/
[2] Arts, N. J., Walvoort, S. J., & Kessels, R. P. (2017). Korsakoff’s syndrome: a critical review. Neuropsychiatric Disease and Treatment, 13, 2875-2890. – https://pubmed.ncbi.nlm.nih.gov/29225466/
[3] National Institute on Alcohol Abuse and Alcoholism. Wernicke-Korsakoff Syndrome. – https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/wernicke-korsakoff-syndrome
[4] Subramanya, S. B., Subramanian, V. S., & Said, H. M. (2010). Chronic alcohol consumption and intestinal thiamin absorption: effects on physiological and molecular parameters of the uptake process. American Journal of Physiology-Gastrointestinal and Liver Physiology, 299(1), G23-G31. – https://pmc.ncbi.nlm.nih.gov/articles/PMC2904112/
[5] Vasan, S., & Kumar, A. (2023). Wernicke Encephalopathy. In StatPearls. StatPearls Publishing. – https://www.ncbi.nlm.nih.gov/books/NBK470344/?report=reader