Phencyclidine (PCP), also known as ‘angel dust,’ was initially developed as an anesthetic in the 1950s but was later banned due to its severe side effects and high potential for addiction. According to the study “Hallucinogens and Dissociative Drugs” by the National Institute on Drug Abuse (NIDA) in 2020, PCP is usually smoked, snorted, injected, or swallowed and causes significant brain damage, leading to hallucinations, delusions, and violent behavior.
The signs of PCP addiction include intense cravings for the drug, loss of control over its use, and continued use despite harmful consequences. Additional signs include aggressive or violent behavior, social withdrawal, and neglect of responsibilities.
The causes of PCP addiction include genetic predisposition, environmental factors, mental health disorders, and peer pressure. The desire for altered perceptions or escape from reality also contributes to the onset of addiction.
The effects of PCP addiction include severe cognitive impairments, respiratory issues, and increased risk of accidents or injuries due to impaired judgment. Psychologically, it leads to paranoia, severe anxiety, and delusions. Socially, addiction results in strained relationships, legal problems, and financial instability.
What Is Phencyclidine?
Phencyclidine (PCP) is a powerful hallucinogen that was initially developed for medical use as an anesthetic. However, due to its severe neurotoxic effects, including intense hallucinations and violent behavior, it was discontinued for medical use. According to the study “Hallucinogens and Dissociative Drugs” by the National Institute on Drug Abuse (NIDA) in 2020, PCP causes users to experience significantly distorted perceptions of reality, making it a dangerous and highly addictive substance.
What Is Phencyclidine Addiction?
Phencyclidine (PCP) addiction is characterized by a compulsive need to use the drug despite its harmful effects. This addiction leads to increased tolerance, requiring more of the drug to achieve the same effect, and physical dependence, where withdrawal symptoms occur without the drug. PCP addiction severely impacts mental health, causing hallucinations, paranoia, and delusions.
Users often engage in risky behaviors, neglect responsibilities, and withdraw socially. According to the National Institute on Drug Abuse, these behaviors pose significant risks to health and safety, necessitating immediate intervention and treatment. Effective treatment includes medical detox, behavioral therapies, and strong support networks.
What Are the Signs of PCP Addiction?
Phencyclidine (PCP) addiction leads to noticeable changes in how a person feels physically, how they act, and their mental state. Recognizing these signs early is crucial for obtaining the right help and treatment. According to the study “Phencyclidine (PCP) Addiction: Signs, Treatment, and Prevention” by Sharp and Graeven, published in 2020, PCP addiction results in a wide range of symptoms, including physical changes such as slurred speech and loss of coordination, behavioral changes like aggression and neglect of responsibilities, and severe psychological symptoms such as hallucinations and paranoia.
These signs disrupt daily life, harm relationships, and endanger personal safety. Understanding the specific manifestations of PCP addiction helps in identifying and addressing the problem promptly.
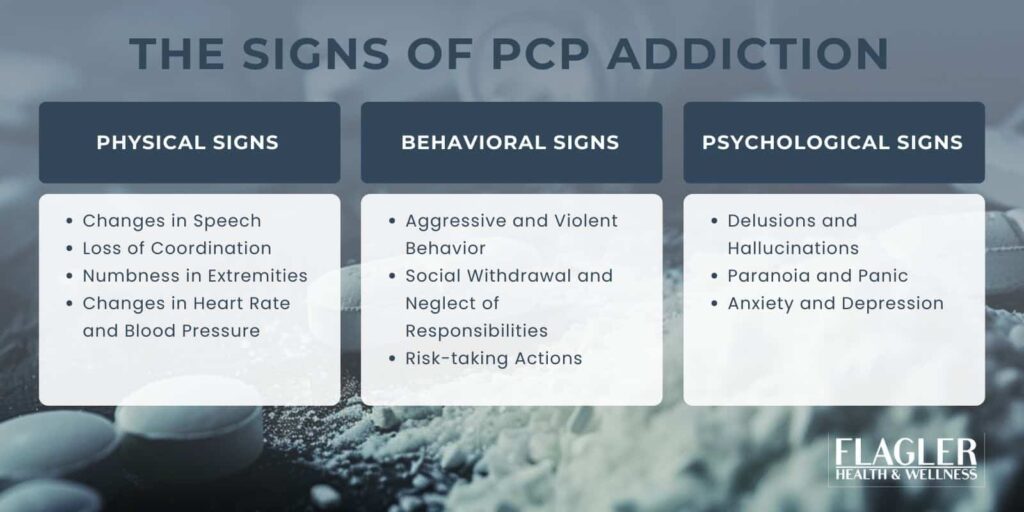
Physical Signs of PCP Addiction
Physical signs of PCP addiction include:
- Changes in Speech: Slurred or incoherent speech hinders communication, making it difficult for the individual to convey thoughts clearly.
- Loss of Coordination: Affected individuals often struggle with balance and coordination, leading to frequent falls or unsteady movements that can result in injuries.
- Numbness in Extremities: PCP causes numbness in the hands and feet, reducing sensitivity and impairing motor functions.
- Changes in Heart Rate and Blood Pressure: The drug induces rapid heart rate (tachycardia) or dangerously low blood pressure, which can lead to cardiovascular complications.
Behavioral Changes of PCP Addiction
Behavioral signs of PCP addiction include:
- Aggressive and Violent Behavior: PCP users become highly aggressive, posing a danger to themselves and others through unpredictable and violent actions.
- Social Withdrawal and Neglect of Responsibilities: Addiction leads to neglect of work, school, and family obligations, resulting in isolation and deteriorating relationships.
- Risk-taking Actions: Engaging in risky activities like driving or operating machinery while under the influence is common, increasing the risk of accidents and injuries.
Psychological Symptoms of PCP Addiction
Psychological signs of PCP addiction include:
- Delusions and Hallucinations: PCP causes users to experience vivid hallucinations and false beliefs, distorting their perception of reality and leading to dangerous behavior.
- Paranoia and Panic: Intense fear and irrational suspicion of others are frequent symptoms, contributing to social withdrawal and erratic behavior.
- Anxiety and Depression: Chronic PCP use leads to persistent anxiety and depressive episodes, severely impacting mental health and overall well-being.
Recognizing these signs early helps individuals seek timely medical intervention and treatment to mitigate the severe health and social consequences of PCP addiction. Understanding these symptoms enables family members, friends, and healthcare professionals to identify PCP addiction and encourage effective intervention.
What Are the Causes of PCP Addiction?
Phencyclidine (PCP) addiction is caused by a combination of brain chemistry, genetics, psychology, and environmental factors. The drug affects brain function by altering neurotransmitter systems, particularly NMDA and dopamine receptors.
According to the study “Common Comorbidities with Substance Use Disorders” by the National Institute on Drug Abuse (NIDA) in 2020, individuals with a family history of addiction are at higher risk for developing substance use disorders. Additionally, mental health issues such as depression and anxiety also contribute to the risk, as people may use PCP as a form of self-medication.
Understanding these intertwined factors is essential for effective prevention and treatment strategies.

How PCP Affects Brain Chemistry:
- Interaction with NMDA and Glutamate Receptors: PCP disrupts normal brain function by blocking NMDA (N-methyl-D-aspartate) receptors and altering glutamate activity, leading to dissociation and hallucinations.
- Dopamine and Opioid Receptor Influence: PCP increases dopamine release, stimulating the brain’s reward system and creating a strong sense of euphoria. It also interacts with opioid receptors, enhancing the addictive potential.
Genetic and Psychological Factors of PCP Addiction:
- Family History of Substance Use Disorders: Individuals with a family history of substance abuse are at higher risk of developing PCP addiction.
- Co-occurring Mental Health Conditions: Depression, anxiety, and other mental health disorders make individuals more susceptible to substance use as a form of self-medication.
Social and Environmental Influences of PCP Addiction:
- Peer Pressure and Availability of PCP: Social circles where PCP use is normalized increase the likelihood of experimentation and eventual addiction.
- Socioeconomic Factors and Exposure to Drug Abuse: Living in environments with prevalent drug abuse or experiencing socioeconomic hardships drives individuals toward PCP use.
How Does PCP Addiction Affect Individuals and Society?
PCP’s ability to alter perceptions and induce a detached state leads to behaviors that threaten personal health and damage relationships. This addiction wreaks havoc on both personal and societal levels, as those affected grapple with the drug’s immediate and long-term powerful effects.
Personal Impact of PCP Addiction:
In the short term, PCP users often experience intense euphoria and a dissociative state that leaves them detached from reality. Their eyes display rapid movements, accompanied by a blank stare, indicative of their altered perception. However, the long-term consequences are far more severe.
Prolonged use leads to significant memory loss and cognitive impairment, impairing users’ ability to function in daily life. They also develop severe depression and unhealthy weight loss due to the drug’s toll on their physical and mental health. Tragically, many long-term users struggle with suicidal thoughts and behavior as their mental health deteriorates further.
Societal Impact of PCP Addiction:
The effects of PCP addiction extend beyond the individual, rippling through society in several ways.
- Violent Crime and Accidents: PCP’s association with heightened aggression and violent behavior contributes to an increase in violent crimes and fatal accidents.
- Healthcare Burden: Emergency room visits due to PCP intoxication strain healthcare resources, as users often require intensive care for violent outbursts and mental health crises.
- Economic Costs: Addiction-related absenteeism, legal issues, healthcare expenses, and law enforcement efforts impose a significant economic burden on society.
- Public Safety Risks: Aggressive and unpredictable behavior by individuals under the influence of PCP poses significant risks to bystanders and first responders.
- Child Welfare Issues: Parental PCP addiction leads to child neglect or abuse, resulting in an increased need for social services and foster care.
Effective prevention and treatment are important factors for mitigating the impact of PCP addiction on individuals and society. Raising awareness through public campaigns, providing strong support networks, and enforcing relevant laws help reduce the harmful effects of PCP addiction. Early intervention programs, mental health services, and family support empower individuals to regain control and lessen the wider societal impact.
What Treatment Options Are Available for PCP Addiction?
Treating Phencyclidine (PCP) addiction is particularly challenging due to the drug’s powerful effects and the potential for violent behavior in users. It requires a multi-faceted approach that addresses both the physical and psychological aspects of addiction. This comprehensive treatment strategy involves several stages and methodologies to ensure a safe and effective recovery. Here’s an overview of the available treatment options:
1. Detoxification and Medical Management
Detoxification is the first step in treating PCP addiction. It involves clearing the drug from the user’s system under medical supervision. In cases of severe PCP reactions or overdoses, immediate medical care in an emergency room is necessary. Medical professionals focus on stabilizing vital signs, reducing fever, and managing agitation with sedation. Common withdrawal symptoms like muscle tremors, diarrhea, and seizures require close monitoring to ensure safe detoxification.
2. Behavioral Therapies
Behavioral therapies are essential in addressing the psychological aspects of PCP addiction. Cognitive-behavioral therapy (CBT) helps individuals identify and change harmful behaviors by teaching coping strategies like meditation and stress management. Contingency Management uses positive reinforcement to encourage sobriety by providing rewards for drug-free urine tests. Motivational Enhancement Therapy (MET) helps individuals find personal motivation to quit by exploring their goals and values.
3. Support Networks
Support networks play a vital role in recovery. Programs like Narcotics Anonymous (NA) offer a supportive community for those in recovery, while Al-Anon provides support for family members affected by a loved one’s PCP addiction. Peer support and family therapy help rebuild trust and provide a strong support system.
4. Rehabilitation Programs
Rehabilitation programs vary based on the intensity and structure of treatment. Inpatient rehabilitation is ideal for those needing intensive, round-the-clock care and therapy. Outpatient rehabilitation offers flexibility for those who need treatment while maintaining their daily responsibilities. Complementary therapies like art therapy and mindfulness meditation help individuals manage cravings and emotional regulation by encouraging creative expression and reducing stress.
Key Points to Remember:
- No Specific Medication: There’s no specific medication to counteract PCP’s effects. Medical professionals focus on managing symptoms and supporting recovery.
- Importance of Support: Connecting with support networks and finding reliable therapy is important for a successful recovery.
- Seek Professional Help: Always consult healthcare professionals or addiction specialists for proper guidance.
According to the report “Highlights of the 2011 Drug Abuse Warning Network (DAWN) Findings on Drug-Related Emergency Department Visits” by the Substance Abuse and Mental Health Services Administration (SAMHSA), 75,538 emergency room visits were linked to PCP, with 72% of these cases involving other substances.
This demonstrates the need for holistic rehabilitation programs addressing co-occurring substance use and mental health issues. With a structured plan that includes detoxification, therapy, and support, individuals struggling with PCP addiction achieve lasting recovery and regain control over their lives.
With a structured plan that includes detoxification, therapy, and support, individuals struggling with PCP addiction achieve lasting recovery and regain control over their lives.
How Can PCP Addiction Be Prevented?
Preventing Phencyclidine (PCP) addiction requires a comprehensive approach involving public awareness, education, and legislation. According to the study “Prevention Strategies for Drug Abuse” by Sharp and Graeven in 2020, effective prevention strategies must address the social and economic factors contributing to drug abuse, emphasizing the need for comprehensive community support and resources. Public health campaigns highlight the dangers of PCP misuse and its severe health and social consequences.
Early intervention programs in schools and community organizations support at-risk individuals. Prescription monitoring programs detect early signs of abuse. Community-based initiatives like peer support networks reduce stigma and encourage help-seeking. Legislation restricting access to PCP-related chemicals and fostering collaboration ensures comprehensive strategies to curb PCP addiction.
Key strategies include:
- Public Awareness Campaigns: Educate people on the dangers of PCP misuse through media, community events, and educational materials to increase awareness and understanding.
- Early Intervention Programs: Identify and support at-risk individuals through school-based programs and community outreach, offering counseling and resources to prevent PCP use.
- Prescription Monitoring Programs: Track trends and detect abuse by monitoring prescriptions, enabling timely intervention when irregularities are detected.
- Community-Based Initiatives: Peer support networks and screening programs within communities help reduce stigma and provide ongoing support for those seeking help.
- Legislative Measures: Restrict access to PCP-related chemicals, improve collaboration between agencies, and enforce laws to prevent the production and distribution of PCP effectively.
Addressing the social and economic factors contributing to PCP abuse is essential. By combining education, community support, and regulation, society significantly reduces the impact of PCP addiction.
How does PCP affect the brain?
Phencyclidine (PCP) primarily affects the brain by acting as an NMDA receptor antagonist, which disrupts normal communication between nerve cells. This interference alters neurotransmitter levels, particularly dopamine and serotonin, leading to distorted perceptions, hallucinations, and mood changes. The drug also induces dissociation, causing users to feel detached from their bodies and surroundings.
What are the risks of mixing PCP with other substances?
Mixing PCP with other substances significantly increases the risk of adverse effects. When combined with depressants like alcohol or benzodiazepines, it leads to respiratory depression and coma. Mixing PCP with stimulants like cocaine or methamphetamine results in severe agitation, paranoia, and violent behavior. Combining PCP with other hallucinogens intensifies delusions and hallucinations, increasing the likelihood of risky behaviors. What are the risks of mixing PCP with other substances?
Can PCP addiction be treated at home?
Due to the drug’s intense withdrawal symptoms and potential for violent behavior, treating PCP addiction at home is not advisable. Withdrawal often includes agitation, muscle breakdown, seizures, and suicidal thoughts. Medical detoxification and professional supervision are necessary to ensure a safe withdrawal and provide comprehensive treatment.
What are the signs of a PCP overdose?
- Uncontrolled muscle movements or seizures
- Rapid heart rate or dangerously low blood pressure
- Respiratory depression or shallow breathing
- Extreme paranoia or violent behavior
- Loss of consciousness or coma
Immediate medical attention is essential if these symptoms occur.
How can families support a loved one struggling with PCP addiction?
Families can support a loved one struggling with PCP addiction by:
- Encouraging them to seek professional treatment
- Avoiding judgmental language and being supportive
- Educating themselves about PCP addiction and treatment options
- Attending family therapy sessions to build a supportive environment
- Establishing healthy boundaries and avoiding enabling behaviors
Are there any medications specifically approved for treating PCP addiction?
Currently, no medications are specifically approved to treat PCP addiction. Treatment focuses on behavioral therapies like Cognitive-Behavioral Therapy (CBT) and Motivational Enhancement Therapy (MET).
What are the potential risks of combining PCP with other substances like hydrocodone, and how should treatment address these complexities?
Combining PCP with other substances like hydrocodone poses significant health risks due to the unpredictable and potentially dangerous interactions between these drugs. PCP’s dissociative effects can be exacerbated by hydrocodone’s depressant properties, leading to severe respiratory depression, heightened hallucinations, and increased risk of overdose. Treatment for individuals using multiple substances must address these complexities through a comprehensive approach that includes medical detoxification, continuous monitoring, and integrated behavioral therapies.
How can prevention strategies for PCP addiction be tailored to address both the unique dangers of PCP and the broader issues of substance use?
Prevention strategies for PCP addiction must address both the specific dangers associated with PCP use and the broader issues of substance abuse. Education campaigns that highlight the severe psychological and physical effects of PCP, including its potential for causing violent behavior and long-term cognitive impairment, can deter use. Additionally, community programs that promote healthy lifestyle choices, provide support for mental health issues, and offer alternatives to drug use can help prevent initial experimentation with substances.
What are the long-term effects of PCP use?
Long-term use of PCP leads to severe health issues, significantly impacting both mental and physical health. These effects include:
- Persistent speech difficulties like stuttering or slurred speech
- Memory loss and cognitive impairment
- Severe depression and anxiety
- Chronic hallucinations and delusions (flashbacks)
- Suicidal thoughts and behavior
- Increased risk of violent behavior and self-harm
Is PCP addictive after one use?
While PCP may not lead to immediate addiction after a single use, its powerful hallucinogenic and dissociative effects increase the risk of developing dependence. Users quickly develop a tolerance, requiring larger doses to achieve the same effects, which leads to a higher risk of addiction.
How long does PCP stay in your system?
The detection time for PCP varies based on usage and the type of test:
- Urine Test: Up to 7-14 days for occasional users; longer for chronic users
- Blood Test: Typically detectable for 1-3 days
- Saliva Test: Detectable for 1-5 days
- Hair Test: Up to 90 days or longer
Detection times vary based on individual metabolism, frequency of use, and dosage.