Table of Contents
Introduction
The streets have a new predator, and it goes by many names—tranq, zombie drug, the sleep-cut. Yet behind these ominous monikers lies a substance originally designed for veterinary use that has now infiltrated America’s drug supply with devastating consequences. Understanding what xylazine is and recognizing its dangers could be the difference between life and death for someone you love.
What Is Xylazine?
Xylazine is a non-opioid sedative originally developed for veterinary medicine, primarily used as a tranquilizer for horses and other large animals. This pharmaceutical compound, often referred to by its street name “tranq,” has never been approved for human use by the FDA. Nevertheless, it has emerged as a dangerous adulterant in the illicit drug market, particularly when mixed with fentanyl and other opioids [1].
The xylazine meaning extends beyond its clinical definition. On the streets, this horse tranquilizer drug represents a growing crisis that’s reshaping America’s overdose landscape. According to the National Institute on Drug Abuse (NIDA), xylazine has been increasingly detected in drug overdose deaths across the United States, particularly in the Northeast and spreading westward [1].
What Is Xylazine Used For?
In its intended veterinary context, xylazine serves as a sedative, muscle relaxant, and analgesic for animals. Veterinarians commonly administer it before surgical procedures or examinations. However, what is xylazine used for in humans differs dramatically from its legitimate medical applications—and that’s where the danger begins.
Drug dealers have discovered that mixing xylazine with opioids like fentanyl extends the duration of the high while reducing production costs. Consequently, users often consume xylazine without knowing it’s present in their drugs. This deceptive practice has transformed xylazine from a veterinary medication into a street drug that’s claiming lives across the nation.
Effects of Xylazine
The effects of xylazine on the human body mirror its impact on animals but with far more dangerous consequences. When consumed, this tranquilizer drug produces profound sedation that can last for hours. Users typically experience extreme drowsiness, slowed breathing, and dangerously low blood pressure. Moreover, the sedative effects can be so intense that individuals appear unconscious or “zombie-like”—hence one of its chilling street names.
What does xylazine do to humans goes beyond simple sedation. The substance affects both the central and peripheral nervous systems, leading to a cascade of physiological responses. Respiratory depression becomes particularly concerning, especially when combined with opioids. Furthermore, the cardiovascular system takes a significant hit, with bradycardia (slow heart rate) and hypotension (low blood pressure) posing immediate threats to survival.
How Does Xylazine Affect the Mind and Body?
The mental and physical toll of xylazine creates a perfect storm of impairment. Neurologically, this tranquilizer for humans induces dissociation, confusion, and altered consciousness. Users often report feeling detached from their bodies, experiencing time distortion, and struggling with memory formation during intoxication.
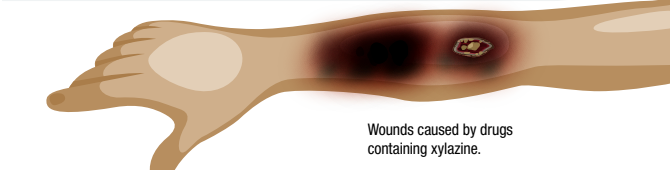
Physically, the xylazine effect manifests through multiple organ systems. Additionally, one of the most distinctive and horrifying consequences involves severe skin wounds. Unlike typical injection site infections, xylazine-related wounds develop into necrotic lesions that can occur anywhere on the body—not just at injection sites. These wounds resist standard treatment protocols and frequently require extensive medical intervention [5].
The Drug Enforcement Administration (DEA) has reported that xylazine mixed with fentanyl creates a particularly lethal combination, as the sedative properties of xylazine compound the respiratory depression caused by opioids [2]. Therefore, users face a doubled risk of fatal overdose when consuming these substances together.
Is Xylazine Addictive? Do People Experience Xylazine Withdrawal?
While research on xylazine addiction in humans remains limited, emerging evidence suggests that physical dependence can develop. People who use xylazine regularly report experiencing withdrawal symptoms when they stop, including anxiety, restlessness, and intense drug cravings. However, the xylazine withdrawal syndrome differs from opioid withdrawal in several key ways.
Unlike benzodiazepines or barbiturates, xylazine is not a benzo, despite producing similar sedative effects. Its pharmacological profile as an alpha-2 adrenergic agonist sets it apart from other drug classes. Consequently, treatment protocols for xylazine addiction must address its unique mechanisms of action while simultaneously managing any co-occurring opioid dependence.
Dangers of Using Opioids Mixed with Xylazine
The xylazine fentanyl combination has become increasingly prevalent, creating what experts call a “perfect storm” of overdose risk. When these substances combine, they produce synergistic effects that dramatically increase the likelihood of fatal outcomes. The DEA has issued widespread alerts about this dangerous trend, noting that xylazine appears in approximately 23% of fentanyl-related deaths in some regions [2].
| Risk Factor | Opioids Alone | Opioids + Xylazine |
| Respiratory Depression | High | Extremely High |
| Naloxone Response | Effective | Partially Effective |
| Wound Development | Rare | Common (40-50%) |
| Recovery Complexity | Moderate | Severe |
What makes this combination particularly insidious is that naloxone (Narcan) cannot reverse xylazine’s effects. While naloxone effectively counteracts opioid overdose, it leaves xylazine’s sedative and cardiovascular effects untouched. As a result, individuals who receive naloxone may regain consciousness from opioid reversal but remain dangerously sedated from xylazine [3].
What Substances Has Xylazine Been Found In?
The xylazine crisis has expanded beyond fentanyl contamination. Testing reveals that this veterinary tranquilizer has infiltrated multiple illicit substances across the drug supply. Cocaine, heroin, methamphetamine, and counterfeit prescription pills have all tested positive for xylazine in various regions. This widespread adulteration means that virtually anyone using illicit substances faces potential xylazine exposure, regardless of their drug of choice.
Maryland’s health authorities have documented xylazine’s presence in diverse drug samples, emphasizing that users cannot determine whether their substances contain this dangerous additive through visual inspection or taste [3]. Therefore, the only way to truly avoid xylazine exposure is to abstain from illicit drug use entirely or seek professional treatment.
Can You Overdose on Xylazine?
Absolutely. Xylazine overdose represents a medical emergency requiring immediate intervention. The substance’s profound effects on respiration and cardiovascular function can prove fatal, particularly when combined with opioids. Moreover, the sedation produced by xylazine can last significantly longer than opioid-induced effects, creating extended periods of vulnerability.
Symptoms of xylazine overdose include extreme sedation, pinpoint pupils, shallow breathing, blue-tinged skin, loss of consciousness, and dangerously low blood pressure. In addition, the risk escalates when individuals consume unknown quantities or when xylazine is mixed with multiple substances—a common occurrence in today’s contaminated drug supply.
What Is Xylazine’s Role in the Overdose Crisis?
The xylazine crisis represents a disturbing evolution in America’s ongoing battle with substance use disorders. This street drug has fundamentally altered the overdose landscape, complicating rescue efforts and treatment protocols. Public health officials have labeled xylazine an “emerging threat” due to its rapid spread and the challenges it poses to traditional harm reduction strategies [1].
States like Pennsylvania have witnessed particularly devastating impacts, with xylazine detected in over 90% of opioid-related deaths in some counties. Furthermore, the geographic spread continues expanding, with western states now reporting increasing xylazine-related incidents. This westward migration suggests that the crisis will intensify before it improves.
How Can I Help Someone Who May Be Experiencing an Overdose Involving Xylazine?
Responding to a suspected xylazine overdose requires swift action, even though the standard opioid reversal protocols prove only partially effective. First, call 911 immediately—professional medical intervention is essential. While waiting for emergency services, take these critical steps:
Administer naloxone if available, as it will reverse any opioid effects present. However, remember that naloxone won’t counteract xylazine’s sedative properties. Additionally, place the person in the recovery position (on their side) to prevent aspiration if they vomit. Monitor their breathing closely and be prepared to perform rescue breathing if respiration becomes critically shallow or stops [4].
Oregon’s health guidelines emphasize the importance of staying with the person until help arrives, as xylazine’s prolonged sedation means they may need extended monitoring and support [4]. Never leave someone alone if you suspect they’ve overdosed on any substance, including those potentially containing xylazine.
How Do You Treat Xylazine-Related Wounds?
Xylazine wound management presents unique challenges that require specialized medical attention. These necrotic lesions differ significantly from typical injection site infections and demand aggressive treatment protocols. Oregon’s Department of Health has developed comprehensive guidelines specifically addressing this growing concern [5].
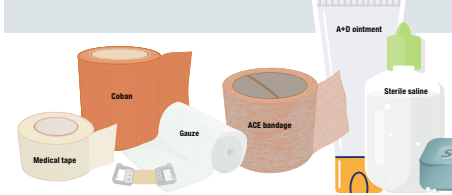
Treatment typically involves:
- Early recognition and assessment by medical professionals
- Aggressive wound cleaning and debridement of dead tissue
- Antibiotic therapy to prevent or treat secondary infections
- Pain management strategies
- Possible surgical intervention for severe cases
- Ongoing wound care and monitoring
Importantly, individuals with xylazine-related wounds should seek medical attention immediately rather than attempting self-treatment. These wounds progress rapidly and can lead to life-threatening complications including sepsis, amputation, or death if left untreated.
Is Xylazine Legal?
The legal status of xylazine occupies a gray area that’s rapidly evolving. While xylazine remains legal for veterinary use, several states have begun classifying it as a controlled substance due to its role in the overdose crisis. The federal government has designated xylazine as an “emerging drug threat,” and regulatory action continues developing at both state and federal levels [2].
Possession of xylazine without legitimate veterinary authorization may carry legal consequences in jurisdictions that have enacted specific legislation. Nevertheless, the primary concern isn’t legal status but rather the life-threatening risks this substance poses. At Flagler Health & Wellness, we focus on treatment and recovery rather than punishment, understanding that addiction is a medical condition requiring compassionate, evidence-based care.
Frequently Asked Questions
Can naloxone reverse a xylazine overdose?
Naloxone (Narcan) cannot reverse xylazine’s effects directly. However, it should still be administered if an overdose is suspected, as most xylazine exposures occur in combination with opioids. Naloxone will reverse the opioid component while emergency services address the xylazine sedation.
How long does xylazine stay in your system?
Xylazine’s effects can last anywhere from 4 to 8 hours, though this varies based on dose, individual metabolism, and other substances consumed. Detection in drug tests may be possible for several days after use, depending on the testing method employed.
Why do xylazine wounds appear all over the body, not just at injection sites?
Unlike typical injection site injuries, xylazine causes systemic vascular damage that can manifest as wounds anywhere on the body. The substance affects blood flow and tissue perfusion throughout the body, leading to necrosis in areas far from injection sites.
Is xylazine the same as ketamine?
No. While both are used as veterinary anesthetics and produce dissociative effects, they belong to different drug classes with distinct mechanisms of action. Xylazine is an alpha-2 adrenergic agonist, whereas ketamine is an NMDA receptor antagonist.
Can someone develop tolerance to xylazine?
Yes. Regular xylazine use can lead to tolerance, meaning individuals require increasing amounts to achieve the same effects. This tolerance, combined with the unpredictable potency of street drugs, significantly increases overdose risk.
Finding Hope and Healing at Flagler Health & Wellness
The emergence of xylazine in the drug supply represents a formidable challenge, but it’s not insurmountable. Recovery is possible, and at Flagler Health & Wellness, we’re equipped to help individuals navigate the complexities of xylazine-involved substance use disorders. Our comprehensive treatment approach addresses the unique challenges posed by this dangerous adulterant while providing the support, medical care, and evidence-based therapies necessary for lasting recovery.

If you or someone you love is struggling with substance use—whether involving xylazine, fentanyl, or other drugs—please know that help is available. The path to recovery begins with a single step, and our compassionate team stands ready to walk alongside you every step of the way. Don’t let fear or shame prevent you from reaching out. Contact us today, your life has value and recovery is within reach.
Sources
[1] National Institute on Drug Abuse. (n.d.). Xylazine. https://nida.nih.gov/research-topics/xylazine
[2] Drug Enforcement Administration. (2022). DEA Reports Widespread Threat of Fentanyl Mixed with Xylazine. https://www.dea.gov/alert/dea-reports-widespread-threat-fentanyl-mixed-xylazine
[3] Maryland Department of Health. (n.d.). Xylazine Information. https://stopoverdose.maryland.gov/xylazine/
[4] Washington County Public Health. (n.d.). Xylazine (Tranq) Information. https://www.washingtoncountyor.gov/addictions/documents/xylazine-tranq-information/download?inline
[5] Oregon Health Authority. (n.d.). Individual Xylazine Wound Management Guidelines. https://www.oregon.gov/oha/PH/PREVENTIONWELLNESS/SUBSTANCEUSE/OPIOIDS/Documents/200-299810_Individual%20Xylazine%20Wound%20Management%20Guidelines%20Final.pdf